With more than 63 million people enrolled in January 2020, Medicaid has been one of the major funding sources for medical services and helped numerous people who have limited income and resources access health coverage in the United States.
Reflecting states policies under federal guidance, criteria and methodology for determining the eligibility of Medicaid among states are inconsistent with each other. Said another way, people who are eligible in one state might be rejected by another due to different state legislation. Moreover, the likelihood of qualifying for Medicaid varies substantially by program type. This article would focus on Medicaid types and Medicaid eligibility for seniors over 65 years old. Keep reading to find out more details.
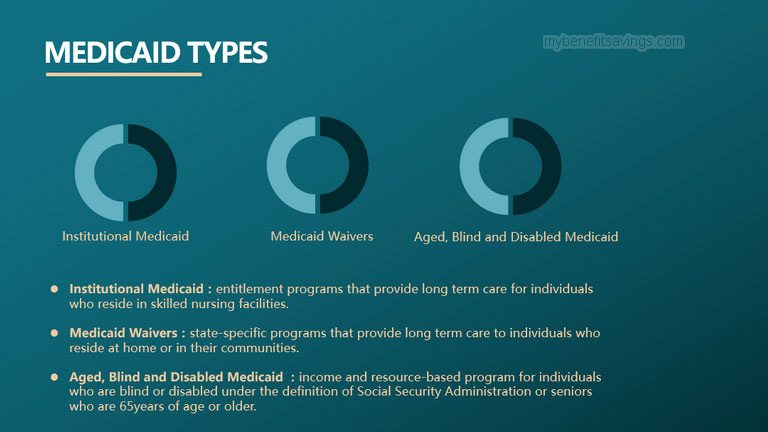
Medicaid Types
Medicaid could be provided in a variety of types. There are basically three types of Medicaid programs that are available in all states.
- Institutional Medicaid
Institutional Medicaid, also known as nursing home Medicaid, is an entitlement program that provides long term care for individuals who reside in skilled nursing facilities. All the applicants would automatically receive Medicaid nursing home care if they meet the eligibility requirements.
- Medicaid Waivers
Medicaid waivers, with a common form of home and community-based services Medicaid waivers, are state-specific programs that provide long term care to individuals who reside at home or in their communities. Since this type of Medicaid is not mandatory, states are allowed to limit the number of enrollees to receive the benefits. Therefore, eligible applicants are often asked to be put on the waiting list for years when enrollment reaches its cap.
- Aged, Blind and Disabled Medicaid
Aged, Blind and Disabled Medicaid, also called regular Medicaid, is an income and resource-based program for individuals who are blind or disabled under the definition of Social Security Administration or seniors who are 65years of age or older.
Medicaid Eligibility
To be eligible for Medicaid, you must firstly fit into a Medicaid eligibility group, which could be broadly classified into mandatory groups and optional groups. Mandatory groups are required by federal statutes and all states must provide Medicaid coverage to qualified individuals under this group.
Part of the Medicaid mandatory populations is listed below:
- Low-income families
- Qualified pregnant women and children
- Individuals receiving Supplemental Security Income (SSI)
You could check all mandatory beneficiary groups by clicking the link below.
https://www.medicaid.gov/sites/default/files/2019-12/list-of-eligibility-groups.pdf
Besides categorically needy groups designated above, states could expand additional Medicaid coverage to optional populations as well. For instance, more than half of states have Medically Needy Programs, allowing people with high medical expenses to “spend down” some of their income so that they could be eligible for Medicaid. Other optional groups also include families with income above federal minimums, individuals at nursing home whose income exceeds SSI limits, the disabled with low-income who need home and community-based care, etc.
Individuals, either in mandatory groups or optional groups, have to meet both financial and functional eligibility to receive Medicaid benefits. However, each state has its discretion to determine Medicaid eligibility criteria. Even in the same state, the eligibility standard could vary by different eligibility groups. Due to this flexibility, it is quite hard to clarify all the eligibility requirements. This article would mainly introduce Medicaid eligibility requirements for seniors over 65 years old.

Financial Eligibility
Incomes and assets are the two main factors considered for financial eligibility purposes. Incomes include your wages, social security benefits, pension payments, interest, dividends from bonds and stocks, estate income, alimony, Veteran’s benefits, IRA distributions, etc. Assets could be divided into exempt assets and non-exempt assets. Exempt assets, literally speaking, are properties that are not counted for the asset test. Up to a specific allowable amount, certain assets such as the home where you live, household furniture and appliances, cars, life insurance policies, funeral, and burial funds are considered to be exempt. On the contrary, non-exempt assets or countable assets including real estate, bank accounts, cash, stocks, and bonds, are properties that are evaluated for your asset test.
All Medicaid programs have income and asset limits for eligibility purposes. From the perspective of applicants’ marital status, it could be classified into limits for individuals and limits for married couples.
- Limited Income
- Individual Income Limit
Stated very clearly, the monthly income limit for individuals is based on 300% of the Federal Benefit Rate (FBR) in most states. Some states also use a percentage of the Federal Benefit Rate (FBR) or the Federal Poverty Level (FPL) to determine individual income limits for Aged, Blind, and Disabled Medicaid. Generally, the single individual income threshold is $2,349 (300% of FBR) per month for nursing home Medicaid or a Medicaid waiver and $783 (100% of FBR) or $1,063 (100% of FPL) per month for Aged, Blind and Disabled Medicaid in 2020.
- Married Applicants Income Limit
Compared to the individual income limit, married applicants’ income limit would be more difficult to calculate. In general, incomes of couples applying for nursing home Medicaid or a Medicaid waiver are required to be counted separately under the instruction of the “Name on the Check Rule”. Each spouse would be considered as an individual applicant for income eligibility. In other words, one spouse’s income could not disqualify another and either husband or wife has an income limit up to $2,349 per month.
Meanwhile, spousal impoverishment rules could protect the community spouse (non-applicant spouse) from becoming impoverished by Minimum Monthly Maintenance Needs Allowance (MMMNA) in the situation with one spouse applying for nursing home Medicaid or a Medicaid waiver. MMMNA is an amount of money that an institutionalized spouse (applicant spouse) transfers to a community spouse from his/her income, allowing the community spouse to reach the minimum income level. And the allocated money would not be counted into the institutionalized spouse’s income eligibility.
Unlike nursing home Medicaid and Medicaid waivers, Aged, Blind and Disabled Medicaid has a different set of requirements on income limit. Combined incomes owned by spouses would be taken as a total income of applicant(s), regardless of whether one or both spouses apply for it. FPL and FBR are often used to determine income eligibility for Aged, Blind and Disabled Medicaid among states. Most states use either 100% of the FPL for a household of two (equal to $1,437 per month) or 100% of the SSI FBR for couples (equal to $1,175 per month). There is no Minimum Monthly Maintenance Needs Allowance permitted for regular Medicaid or Aged Blind and Disabled Medicaid.
- Limited Asset
- Individual Asset Limit
In most states, the asset limit (countable assets) is up to $ 2,000 for single applicants who apply for nursing home Medicaid, Medicaid waivers, or regular Medicaid. There are exceptions as well. States like New York would require a relatively higher limit of up to $15,750.
- Married Applicants Asset Limit
The asset limit (countable assets) in many states for married couples with both spouses applying for nursing home Medicaid or a Medicaid waiver is up to $ 4,000 for two spouses or $ 2,000 for one spouse. In the situation with only one spouse applying for long-term care Medicaid, jointly-owned assets are normally considered as the asset basis of the applicant spouse. However, the community spouse could retain half of the joint assets up to maximum Community Spouse Resource Allowance (CSRA) of $128,640 in most of the states. And to protect those who have limited resources, a minimum CSRA of $25,728 could be kept by a community spouse to ensure his/her daily life needs. Medicaid administrator would deduct the CSRA from the applicant spouse’s countable assets and consider the reduced part as his/her owned asset.
The asset limit (countable assets) for married couples applying for Aged, Blind and Disabled Medicaid is up to $3,000, regardless of whether one or both spouses apply for it. Please also note that there is no CSRA permitted for Aged Blind and Disabled Medicaid.
Below is an example of income and asset limits of Medicaid in Alabama for seniors over 65 years old in 2020. You could find more details about state-specific Medicaid on https://www.medicaid.gov/
| Marital Status | Income Limit | Asset Limit |
| Single | Institutional / Nursing Home Medicaid | |
| $2,349 / month | $2,000 | |
| Medicaid Waivers / Home and Community- Based Services | ||
| $2,349 / month | $2,000 | |
| Regular Medicaid / Aged Blind and Disabled Medicaid | ||
| $803 / month | $2,000 | |
| Married | Institutional / Nursing Home Medicaid | |
| $2,349 / month for each spouse
(Name on the Check Rule) |
One spouse applying:
$2,000 for the applicant spouse $128,640 for the non-applicant spouse |
|
| Both spouses applying:
$ 4,000 for two spouses or $ 2,000 for one spouse |
||
| Medicaid Waivers / Home and Community- Based Services | ||
| $2,349 / month for each spouse
(Name on the Check Rule) |
One spouse applying:
$2,000 for the applicant spouse $128,640 for the non-applicant spouse |
|
| Both spouses applying:
$ 4,000 for two spouses or $ 2,000 for one spouse |
||
| Regular Medicaid / Aged Blind and Disabled Medicaid | ||
| $1,195 / month | $3,000 | |
Functional Eligibility (Medical Eligibility)
“Nursing home level of care”, also known as “nursing facility level of care (NFLOC)” is often used to determine medical eligibility through a person’s physical functional ability, behaviors, medical needs, and cognitive functioning. A list of questions is required to examine a person’s ability to perform Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADL). Applicants must reach a certain score to become medically eligible. However, medical eligibility changes based on Medicaid types, and not all the Medicaid programs require medical eligibility. There is no medical requirement for blind or disabled or seniors (over 65) applying for Aged Blind and Disabled Medicaid while a Level-of-care assessment is needed to evaluate the medical eligibility of people who apply for nursing home Medicaid or Medicaid Waivers.







Leave a Reply